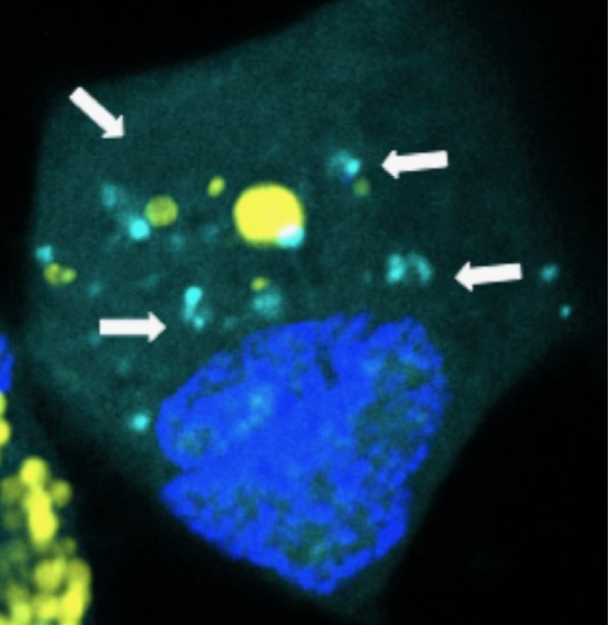
Pictured: Nanoparticles releasing microRNAs inside a brain cancer cell.
Johns Hopkins Kimmel Cancer Center brain cancer researchers announced that they successfully delivered ultra-tiny nano-size packets of genetic code, called microRNAs, in animal models of human brain cancer.
This multi-specialty study was led by John Laterra, M.D., Ph.D., co-director of the Kimmel Cancer Center Brain Cancer Program and Jordan Green, Ph.D., a biomedical engineering and brain cancer expert, and supported, in part, by the Bloomberg~Kimmel Institute for Cancer Immunotherapy.
The researchers say the contents of the super-small containers were designed to target cancer stem cells, a small but relentless population of cellular “seeds” that are able to evade therapy and maintain the growth and spread of tumor cells. Theses cells, along with the blood brain barrier, make it extremely difficult to rid the brain of cancer cells.
The blood brain barrier protects the critical functions of the brain but when it comes to cancer treatment, it is a roadblock that prevents cancer drugs from getting to brain cancer cells.
“Brain cancer is one of the most widely understood cancers in terms of its genetic makeup, but we have yet to develop a good treatment for it,” says Laterra “The resilience of cancer stem cells and the blood-brain barrier are major hurdles.”
He and Green believe their research demonstrates a delivery method to get these microRNAs past the blood brain barrier and into brain cancer stem cells to prevent their ability to sustain the cancer. The nano-packets are made of biodegradable plastic similar to material used for surgical sutures and that degrades over time. They are 1,000 times smaller than the width of a human hair and typical of the size and shape of natural components that cells use to communicate. When cancer cells engulf the packets, they break apart and release their microRNA “payload” specifically where the microRNAs need to take action within the cancer cells. They work by blocking cancer stem cell’s protein-making abilities and turn off programs that drive the cancer cells’ ability to seed new cancer cells and also make cancer cells more susceptible to treatment with drug and radiation therapies.
To illustrate, Green points to glioblastoma, the form of brain cancer that Arizona Sen. John McCain is battling, which often requires repeated surgeries. Doctors remove the brain tumor they can see, but the cancer often returns quickly as unseen cancer cells, such as cancer stem cells, continue to fuel the growth of the cancer says Laterra. As a result, most patients with glioblastoma live less than two years after diagnosis.
“To modernize brain tumor treatments and make progress against brain cancers like glioblastoma, we need tools and methods that bypass the blood-brain barrier and get to cancer stem cells,” says Green. “This type of technology may allow us safely and effectively deliver sensitive genetic medicines directly to tumors without damaging normal tissue.”