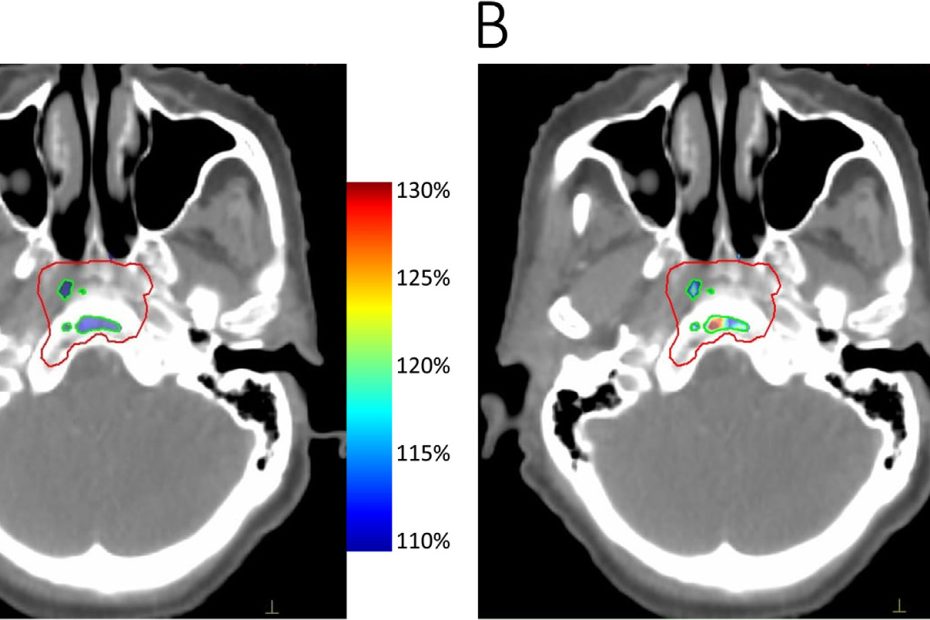
On Target with Dr. Akila Viswanathan – Dr. Kristin Redmond and Brain and Spinal Tumors
In this edition of the On Target podcast, Dr Akila Viswanathan speaks with Dr Kristin Redmond about treating brain and spinal tumors and her research… Read More »On Target with Dr. Akila Viswanathan – Dr. Kristin Redmond and Brain and Spinal Tumors