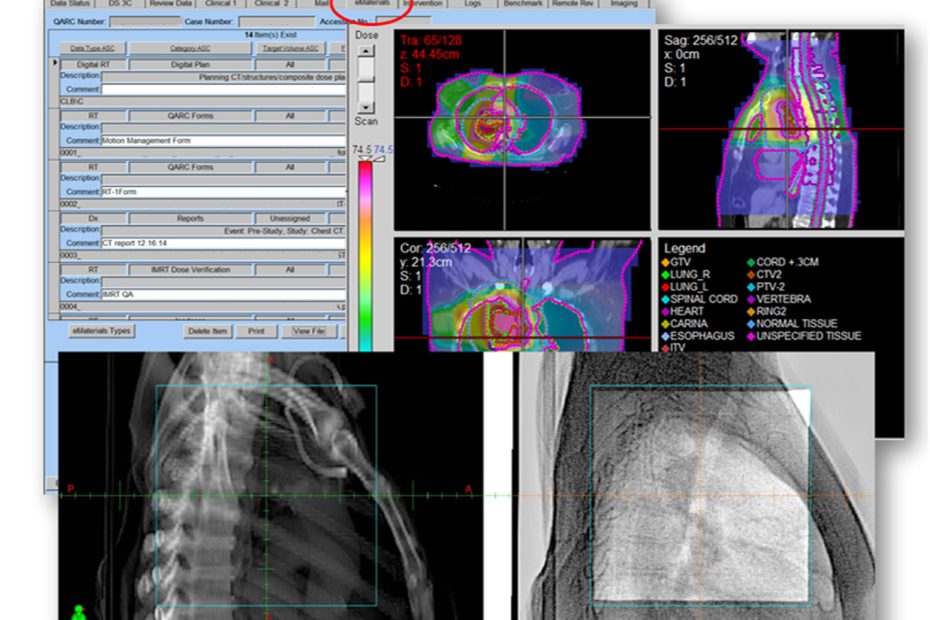
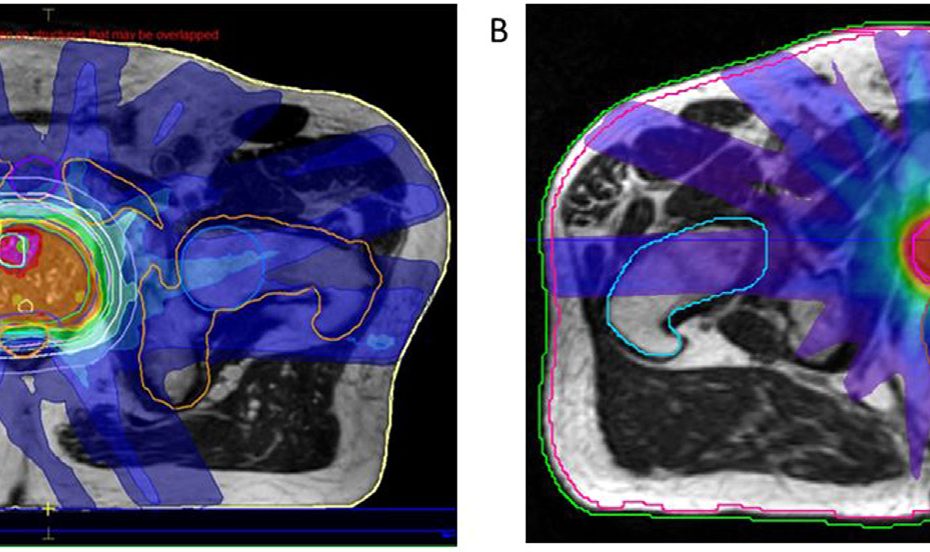
On Target with Dr Akila Viswanathan – Spatially Fractionated and FLASH Radiotherapy for Seminars in Radiation Oncology
In this On Target podcast, Dr Akila Viswanathan talks with Dr Robert Griffin from the University of Arkansas for Medical Sciences and Dr Chandan Guha… Read More »On Target with Dr Akila Viswanathan – Spatially Fractionated and FLASH Radiotherapy for Seminars in Radiation Oncology